I love the *idea* of letting my children explore and experiment with things, permitting they are appropriate and safe. However, I find that the *idea* of letting them do this and the reality of being able to allow it often collide...and explode.
I wish I could allow them to be crafty and NOT CARE that there was glue and glitter and marker all over the kitchen, but I have a house full of 7 people to maintain...plus, who wants to waste money replacing things that get damaged?
I wish I could laugh as they chased each other around the house, SHRIEKING with delight and making my ear drums ring, but, unfortunately, I do not enjoy migraines...plus you can only take so much medication before you're doing more harm than good!
I wish I could let them get FILTHY in the dirt playing outside, catching bugs and picking their nose, but I can't help but tell them to "Keep away from there, in case there's black widows!" or " Please keep those DIRTY fingers out of your mouth...and your sister's!"...plus, I really like to avoid unnecessary exposure to germs and deadly pests, even if SOME germs are a good thing.
I wish I could NEVER have to yell or raise my voice at my children, but if I never did they'd never hear me over their own chorus of cheers, chants and tears...plus, I hear yelling a little keeps you from going off the deep end completely.
I wish that I could say I loved breastfeeding ALL the time because it's only beautiful and wonderful and joyous, but then I'd be not only a liar but discrediting myself and the other moms when they are going through a BAD or DIFFICULT phase...plus, let's face it, after 2.5 years sometimes you just want to say no, because you can.
I wish that I could let my house stay in a constant state of toy mess and not get frustrated at the massive piles of trucks, barbies and stubbed toes that result from it but, I enjoy NOT stubbing my toe to a bloody nubbin and having a neat and organized house that doesn't automatically scream "KIDS LIVE HERE" when someone walks in the door...plus, who really enjoys having bloody nubs for toes?
I really do wish I could live up to the *idea* of that kind of mom, but instead, I'll keep doing my best to reach that point and not cry if I miss it by an inch...or a mile...plus, who REALLY wants to be *perfect* anyhow?
5.14.2010
5.11.2010
Placenta Encapsulation-Phase 2
I posted the first part of the process yesterday and I really hope you learned something you didn't know about placentas and encapsulation of them. After going through this process now, I am eager and excited to help another mama out by offering encapsulation for her. I hope this was useful to you and please, feel free to share this blog with mother's you know to spread the word on the benefits of placenta pills and help someone learn the process.

STEP 11:
After removing the placenta from the oven and letting cool, break larger pieces by snapping them. Pieces should be about 3/4 in.


STEP 12:

Place pieces in grinder (Mr. Coffee works great, but remember, you must only use this grinder for placentas so you'll need one separate from your "regular" coffee grinder). Note that some pieces may not grind down. Larger calcifications or clusters of hardened vessels will simply stay intact, that's ok. Just discard this larger chunks.
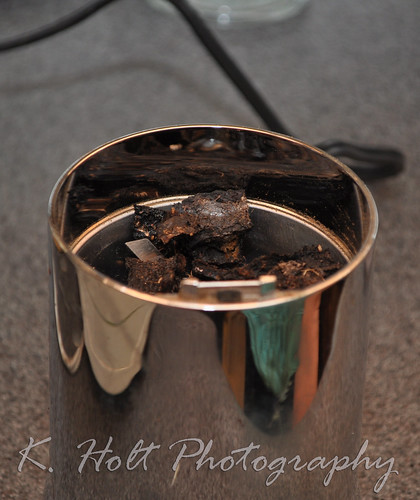
Your ground placenta should look like this:

STEP 13:
Pour all the ground placenta into a bowl or onto a deep plate.

STEP 14:

Take the two parts of your capsules (we used organic vegetarian gelatin capsules, sizes 0 and 00. 0 seemed to work best for me and is a little smaller.) and scoop them towards each other in the freshly ground powder, making sure to seal tightly. Place in "resting place" on paper towel.


STEP 15:
Discard any excess capsules that came in contact with the powder as well as any excess powder that you couldn't encapsulate.

STEP 16:
Wipe down the pills to remove any loose powder, grooved paper towels work great. Then place in jar/bottle/bag to give to mama. Store in fridge or freezer.

We were able to yield 122 good size capsules from this placenta. Mom takes about 3 tablets 2-3 times daily for general use or up to 8 a day if using to stave off post partum depression.

A huge thank you to the lovely Jessica J. for teaching Doula Faye and myself this art of placenta encapsulating. I am happy to offer this service to anyone who might be interested and we'd love to spread the knowledge, know-how and fun of this ancient art.

STEP 11:
After removing the placenta from the oven and letting cool, break larger pieces by snapping them. Pieces should be about 3/4 in.


STEP 12:

Place pieces in grinder (Mr. Coffee works great, but remember, you must only use this grinder for placentas so you'll need one separate from your "regular" coffee grinder). Note that some pieces may not grind down. Larger calcifications or clusters of hardened vessels will simply stay intact, that's ok. Just discard this larger chunks.
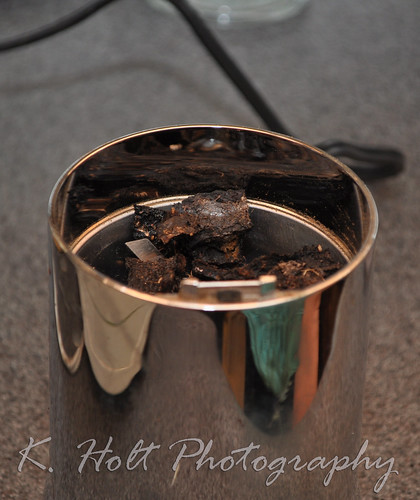
Your ground placenta should look like this:

STEP 13:
Pour all the ground placenta into a bowl or onto a deep plate.

STEP 14:

Take the two parts of your capsules (we used organic vegetarian gelatin capsules, sizes 0 and 00. 0 seemed to work best for me and is a little smaller.) and scoop them towards each other in the freshly ground powder, making sure to seal tightly. Place in "resting place" on paper towel.


STEP 15:
Discard any excess capsules that came in contact with the powder as well as any excess powder that you couldn't encapsulate.

STEP 16:
Wipe down the pills to remove any loose powder, grooved paper towels work great. Then place in jar/bottle/bag to give to mama. Store in fridge or freezer.

We were able to yield 122 good size capsules from this placenta. Mom takes about 3 tablets 2-3 times daily for general use or up to 8 a day if using to stave off post partum depression.

A huge thank you to the lovely Jessica J. for teaching Doula Faye and myself this art of placenta encapsulating. I am happy to offer this service to anyone who might be interested and we'd love to spread the knowledge, know-how and fun of this ancient art.
5.10.2010
Placenta Encapsulation-Phase 1
This is honestly not something I would have ever thought I'd think was beneficial or anything short of freaky. However, the more I learn about pregnancy and childbirth, especially the benefits of natural remedies or alternatives, the more this became a topic of interest. I'm sad now that I never got to examine my placenta much less use it to my advantage health wise. Encapsulation is not consumption in the sense that you're "eating" your placenta. It is the process in which you cook and dry it with herbs and put it in pill form to take post partum.
For more information on the benefits of placenta encapsulation and why many women choose this option (or perhaps to learn of the benefits for yourself) please visit: http://placentabenefits.info/about.asp
What you need:
*Dissection kit (surgical scissors, scalpel, tweezers)
*Sterile Gloves
*Strainer
*Large Pot
*Baking tray
*Oven/dehydrator
You must only use these items for placenta encapsulation. If you're doing this regularly, you need to make sure you have a separate baking tray only for placentas, a separate pot only for placentas, a separate strainer...you get it.
STEP 1:
Wipe placenta clean with gauze or cloth, removing as much blood/debris as possible.

STEP 2:
Remove membrane (sac) with scissors, following the margin of the placenta.

-Puncture hole in membrane with sharp point of scissors and follow along placenta's edge, removing as much as possible. You can try to remove the membrane from the fetal side of the placenta as well.

STEP 3:
Using scissors, remove cord at base.

STEP 4:
Fill pot about 1/2 way with water so that strainer can sit above water level, floating freely without touching the water.
-Grate fresh ginger over placenta, covering lightly.

-Pour ground tea (chai is good, vanilla chai smells heavenly) over placenta, 3-5 bags depending on size.
-squirt with lemon.
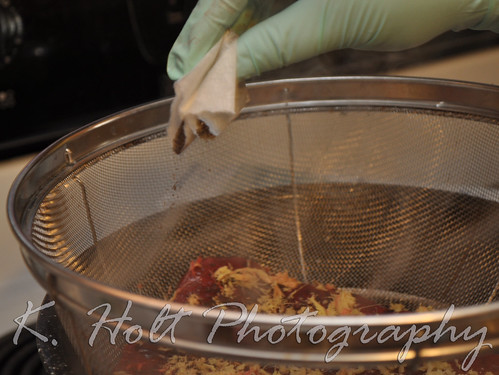
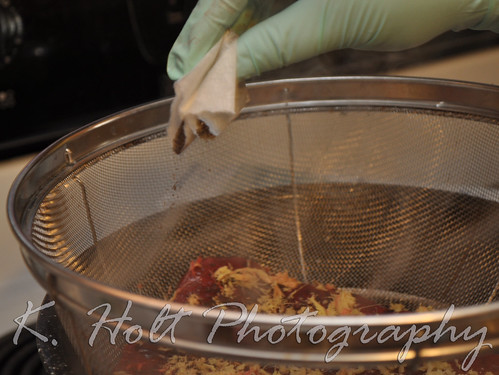
STEP 5:
Place placenta in strainer over water, remember water should not touch placenta.

STEP 6:
Once boiling, let steam for 20 minutes, placenta will shrink.


STEP 7:
Remove steamed placenta from strainer and place on non-stick baking tray.

STEP 8:
With scalpel and tweezers, cut into even strips.


STEP 9:
Arrange evenly on tray to allow air flow.

STEP 10:
Place in oven 200-225 degrees and bake for 8-10 hours.

Pieces should be completely dry, black and not at all rubbery.
***Phase 2 tomorrow!***
This process has been not only fun but VERY informational. The placenta is an AMAZING organ. Something that only begins to grow as life begins and continues to grow with your baby, providing nourishment during your pregnancy. How awesome that it's amazing benefits don't end there? I hope you enjoyed what I've shared so far today and look forward to the rest of the process and sharing that with you tomorrow.
Please post any questions or discussion below.
For more information on the benefits of placenta encapsulation and why many women choose this option (or perhaps to learn of the benefits for yourself) please visit: http://placentabenefits.info/about.asp
What you need:
*Dissection kit (surgical scissors, scalpel, tweezers)
*Sterile Gloves
*Strainer
*Large Pot
*Baking tray
*Oven/dehydrator
You must only use these items for placenta encapsulation. If you're doing this regularly, you need to make sure you have a separate baking tray only for placentas, a separate pot only for placentas, a separate strainer...you get it.
STEP 1:
Wipe placenta clean with gauze or cloth, removing as much blood/debris as possible.

STEP 2:
Remove membrane (sac) with scissors, following the margin of the placenta.

-Puncture hole in membrane with sharp point of scissors and follow along placenta's edge, removing as much as possible. You can try to remove the membrane from the fetal side of the placenta as well.

STEP 3:
Using scissors, remove cord at base.

STEP 4:
Fill pot about 1/2 way with water so that strainer can sit above water level, floating freely without touching the water.
-Grate fresh ginger over placenta, covering lightly.

-Pour ground tea (chai is good, vanilla chai smells heavenly) over placenta, 3-5 bags depending on size.
-squirt with lemon.
STEP 5:
Place placenta in strainer over water, remember water should not touch placenta.

STEP 6:
Once boiling, let steam for 20 minutes, placenta will shrink.


STEP 7:
Remove steamed placenta from strainer and place on non-stick baking tray.

STEP 8:
With scalpel and tweezers, cut into even strips.


STEP 9:
Arrange evenly on tray to allow air flow.

STEP 10:
Place in oven 200-225 degrees and bake for 8-10 hours.

Pieces should be completely dry, black and not at all rubbery.
***Phase 2 tomorrow!***
This process has been not only fun but VERY informational. The placenta is an AMAZING organ. Something that only begins to grow as life begins and continues to grow with your baby, providing nourishment during your pregnancy. How awesome that it's amazing benefits don't end there? I hope you enjoyed what I've shared so far today and look forward to the rest of the process and sharing that with you tomorrow.
Please post any questions or discussion below.
Labels:
midwifery,
natural birth,
placenta,
placenta encapsulation
Solids: The When, What and HOW.
WHEN?
The AAP states that all infants should be exclusively breastfed for 6 months of life and then at least a year or however long is mutually desired.
Many people don't fully understand what "exclusively" breastfeeding means. It means nothing but breastmilk: no formula, no solids.
Why wait 6 months, why not 4?
A baby's digestive tract matures enough for solid foods (those that aren't breastmilk) between 4 and 6 months of age. Waiting until 6 months ensures your baby's digestive tract can tolerate solid foods. Many of the problems associated with early solids do not show up until later in life and many parents and/or doctors never make the association. It's thanks to many years of studies and the advanced knowledge we've gained about infant's bodies that we know waiting the six month MINIMUM is ideal for optimal health, now and in the future.
Another point often left out of the solid discussion is watching for signs of readiness. Just because your baby is 6 months old doesn't mean they are ready, and just because they've met all the signs of readiness doesn't mean you shouldn't wait until they are 6 months old.
Signs that indicate baby is developmentally ready for solids include:
* Baby can sit up well without support.
* Baby has lost the tongue-thrust reflex and does not automatically push solids out of his mouth with his tongue.
* Baby is ready and willing to chew.
* Baby is developing a “pincer” grasp, where he picks up food or other objects between thumb and forefinger. Using the fingers and scraping the food into the palm of the hand (palmar grasp) does not substitute for pincer grasp development.
* Baby is eager to participate in mealtime and may try to grab food and put it in his mouth.
Baby really needs most/all of these stages to be met as WELL as the 6 month minimum age before they're ready for solids.
A reminder: Solids are *only* for exploration and taste in the first year. They do not replace breastmilk, they are not a nutritional supplement to breastmilk and they should always be given AFTER nursing session. Solids are the first step in weaning.
For more information on solids, visit this great link:
http://www.kellymom.com/nutrition/solids/solids-when.html
What have you learned over the years as to how to approach solids? Did you learn anything knew today? What questions might you ask?
WHAT?
Most parents today think the first introduction to food should be fortified rice cereal. Many pediatricians praise that little box of mush. But, how good IS rice cereal, or any cereal, for your little baby?
More on rice cereal: http://www.homemade-baby-food-recipes.com/best-first-food-for-baby.html
You can SKIP the cereal altogether and go for healthy, fresh foods instead. Remember that some foods are unsafe for infants (eggs, peanut butter and milk. Dairy can be added around 9 months old in the form of yogurt, cheese, etc).
Avocado is a great first food as it's mostly bland and high in natural fats, which are important for a developing infant. Many moms will mix breastmilk with their first solid feedings, but it's not necessary. Read your baby, watch for their cues. Let baby take the wheel, too, with exploring solids and don't be afraid of the mess.
Always wait a few days between new foods to watch for possible allergies/reactions and don't over-feed solids.
HOW?
Like I said, let baby take the wheel. Put some food down in front of him/her, sit next to them and watch him explore and enjoy. If baby has met the required milestones for starting solids, then they should be able to pinch and put to mouth any bits of food. If they are unsure of what to do, offer a little taste to intrigue them.
Take it SLOW.
There is no rush to get your baby to eat food. They are getting all the nutrition they need from your milk, this is just for fun and to help them learn so that by about a year old, they are able to eat more meals.
It's always important to listen to your baby, but you have to maintain a sense of responsibility.
Your baby COULD over eat, so don't let them eat more than an ounce or two.
Always wait at LEAST 6 months and make sure all milestones of solids readiness are met.
Avoid known allergens and always watch for reactions no matter what it is you've fed them.
Always wait a few days between trying new foods.
Don't rush, go at your baby's pace.
Have fun!
Labels:
baby,
breast-feeding,
first foods,
food,
infants,
parenting,
solids,
starting foods
5.09.2010
Epidural Epidemic - Drugs in Labor: Are They Really Necessary. . . or Even Safe?
Just had to share this well written, well cited article. I do not hate women for getting epidurals, I hate the cultural fears and over-management of childbirth by Obs and CNMs that has caused them to think they NEED it and led them to LIE on it's safety. Please, take control of your labor and delivery. *Know* the risks of epidurals and other interventions, learn when they ARE necessary and how to avoid them. Look for alternatives to managing pain and labor because they DO exist, they ARE effective and they leave you feeling more positive and accomplished about your birth. It's not a slight against you, it's not an insult to women who've gotten epidurals (I'm ONE of those women!) it's about doing BETTER and becoming more INFORMED for yourself and your baby.
Epidural Epidemic - Drugs in Labor: Are They Really Necessary. . . or Even Safe?
By Joanne Dozer and Shannon Baruth
Issue 95, July/August 1999
The use of epidurals is so common today that many perinatal professionals are calling the 1990s the age of the epidural epidemic. Believed by many in the medical profession to be safe and effective, the epidural seems now to be regarded as a veritable panacea for dealing with the pain of childbirth.
It is true that most women experience pain during the course of labor. This pain can be intense and very real, even for those who have prepared for it. But pain is only one of many possible sensations and experiences that characterize the experience of giving birth. Barbara Katz Rothman, a sociologist who studies birth in America, writes that in the medical management of childbirth, the experience of the mother is viewed by physicians as pain: pain experienced and pain to be avoided.1 Having experienced childbirth ourselves, we have great compassion for women in painful labors. However, we also feel a responsibility to mothers and their babies to explore issues concerning the use of epidural anesthesia in labor issues that are seldom discussed prenatally.
Several factors make the use of epidurals potentially hazardous. The Physician’s Desk Reference cautions that local anesthetics - the type used in epidurals - rapidly cross the placenta. When used for epidural blocks, anesthesia can cause varying degrees of maternal, fetal, and neonatal toxicity which can result in the following side effects: hypotension, urinary retention, fecal and urinary incontinence, paralysis of lower extremities, loss of feeling in the limbs, headache, backache, septic meningitis, slowing of labor, increased need for forceps and vacuum deliveries, cranial nerve palsies, allergic reactions, respiratory depression, nausea, vomiting, and seizures.2 In addition, a piece of the catheter that delivers the drug into the duraregion of the back may break off and be left in the woman, a dangerous risk that necessitates surgical removal. One of the most well-known side effects of spinal anesthesia is a spinal headache. Depending on the amount of anesthetic used and how the catheter was placed, the headache can be mild or severe, lasting between one and ten days after the birth. This is not how any of us wants to feel in our first days and hours with our newborn.
Epidurals also have been linked to an overall increase in operative deliveries: cesareans, forceps deliveries, and vacuum extractions. A meta-analysis of the effects of epidural anesthesia on the rate of cesarean deliveries was undertaken by a group of physicians who examined, categorized, and analyzed all available literature. Eight primary studies revealed that the rate of cesarean section was 10 percentage points higher in the women who had received epidural anesthesia. One study actually found that the cesarean rate increased to 50 percent when the epidural was given at 2 cm dilation, 33 percent at 3 cm, and 26 percent at 4 cm.3 What caused this increase? In the first stage of labor, the muscles of the pelvic floor may become slack from the numbing effects of the epidural, causing the baby to change an otherwise ideal position or fail to descend into the pelvic cavity. In the second stage of labor, the anesthetized woman often is unable to push effectively since she cannot feel her muscles. When the baby does not descend properly or is malpositioned, progress can slow or stop, resulting in a longer labor and the increased possibility of a cesarean section, vacuum extraction, or forceps delivery.
In addition, epidurals usually slow contractions, which prompts medical personnel to administer intravenous Pitocin in order to strengthen them and increase their frequency. Even with Pitocin, which carries its own set of risks, an anesthetized labor may remain prolonged, risking a difficult labor with lack of progress. Prolonged labors put both mother and baby at greater risk of infection, necessitating the use of antibiotics. The longer a labor and slower the progress, the more likely it will end in a forceps, vacuum, or cesarean delivery. Since cesarean section is a major surgery, it strongly influences a woman’s recovery and the initiation of breastfeeding. Of course, the rate of postpartum infection is much higher with cesarean births. All vacuum extraction and forceps deliveries increase the risk of morbidity and birth injuries.
Another effect of epidurals during labor is the creation of hypotension in the mother, which can lead to bradycardia (a decrease in the heart rate) in the fetus. All types of anesthesia, including epidurals, can negatively affect the baby’s heart rate, possibly leading to fetal distress and necessitating an operative delivery. The newborn can continue to have breathing difficulties after birth, requiring supplemental oxygen or even resuscitation. While these problems may be resolved immediately following the birth, they often require the mother to be separated from her baby for neonatal nursery observation. This separation delays bonding and initial feeding. In addition, poor muscle tone and increased acidity in the baby’s blood due to bradycardia and oxygen deprivation may affect her ability to suck effectively, hampering initial attempts at early breastfeeding.
A mother’s temperature may become elevated with the use of epidural anesthesia, resulting in the infant being taken to the nursery and given a full work-up for possible infection. This may include extensive blood work and a spinal tap.4, 5
Furthermore, though epidurals usually remove all sensation in the lower body, "windows" can occur which leave the woman experiencing the intensity of her labor (perhaps on one side of her body) but with extremely limited mobility - obviously hindering her ability to cope with her contractions.6 The idea that pain medication can play a role in "natural childbirth" is deceptive, despite the assurance of the authors of What to Expect When You’re Expecting that "...wanting relief from excruciating pain is natural...therefore pain relief medication can play a role in natural childbirth."7 This is rather twisted logic, since the concept of natural childbirth depends on the mother experiencing both mental and physical sensations of labor. The epidural may allow a woman to be awake and aware of what is happening, but she will not be experiencing a natural labor as she will be numb to any physical sensations below the waist. A split between the mind and the body is effectively created with this anesthetic, disengaging her mind from her physical feelings. Could such disconnection be natural childbirth? Robbie Davis-Floyd, an anthropologist who studies birth in America, argues that the woman in labor with an epidural "...is separated as a person as effectively as she can be from the part of her that is giving birth."8 There is an eerie quality to this kind of birth; the mother is robbed of her own connection to her power and life-creative force. She loses the opportunity to experience the inherent wisdom of the body and its ability to birth without interference. Indeed, most women who have felt childbirth agree that it was a deep, enriching, and positive experience.
What alternatives do women have for the relief of pain in labor? Unfortunately, many women enter the birth experience with a strong belief that birth is something horrible and nightmarish. They are already filled with fear, not only for their own and their baby’s safety but also about what they have heard is the unbearable pain of childbirth. Another important fear is that of "losing control" during labor and delivery. A mother often is labeled out of control if she expresses the natural, primal sounds of labor. Technologically oriented medical practitioners who are sure that childbirth is something to be wrestled into submission feel that the sound of a mother wailing in pain is a sign that she is "losing it" and ought to be medicated. In hospitals, mothers are often told by well-meaning nurses to be quiet so as not to disturb the other "patients." But release of sound is a natural way to express and release painful - and intense - sensations. Suppressing a mother’s natural instincts to move around freely and make noise in labor will increase her actual pain. The prepared childbirth movement - in particular the Lamaze technique - has been successful for some women by helping them remain "in control" by training for structured labor breathing. However, some women actually do connect to their body rhythms and natural breathing patterns in labor, and if they are more loyal to themselves than to their training, they may be seen as wild, out-of-control "Lamaze failures." This failure is defined as their inability in labor to be mannerly and controlled. In fact, one of the primary psychological reasons for lack of progress and cesareans is a fearful mother’s unconscious attempts to control the intensity of her labor. Her lack of progress is due to her inability to let go and surrender. Mothers are told they must be in control when actually they need to let go.
So how does a mother let go and find her way through the pain of labor? First, she needs to give birth where she feels safe. For some women this may mean a medicalized hospital birth; others may feel safest at home or in an alternative birthing center. Most women find that they feel safest in the loving hands of a practitioner with whom they have developed a supportive and loving relationship. This person may be a special kind of doctor or it may be a midwife. Midwives specialize in personalized, supportive perinatal care. Support is the best form and prime source of non-pharmacological pain relief. Support can also come from the love and care of a partner. If you are having your baby in a hospital, it may be worthwhile to secure the help of a knowledgeable friend or a doula. Support can be active: massage, breathing together, encouraging words and attentiveness, and reassurance that what it happening is normal and that you are handling it well. Other support can be more passive: a midwife’s calm demeanor, a gentle nurse’s presence, the peaceful attentions of loved ones. A laboring mother needs to feel safe, loved, and accepted. And when she is, whether she screams, hollers, whines, moans, bargains, begs, or just plain doesn’t act "civilized," giving birth vaginally without medication is a triumph in itself.
One of the ways to endure labor is to recognize (ideally, during one’s prenatal education) the connection between fear, tension, and pain - the "fear-tension-pain syndrome." Basically, when a mother feels fear, she will be tense and experience more pain. Relaxation relieves the tension that helps create the sensation of intense pain. The notion of a relaxing labor might seem crazy, but it is possible, and we have seen it many times. Of course, a mother will feel more relaxed and safer in the birth environment of her choice and with her chosen caregivers. Perhaps the more the mother chooses about her birth environment, the more fully she can relax.
Childbirth education classes that focus on birth as natural and normal encourage women to trust the birthing process. Birthing is full of new sensations which can be frightening and difficult to integrate; some women tell us that they felt they might split in two! Understanding the reasons behind the sensations can make them more manageable, since we fear most that which we do not understand. Another key concept in prenatal education is truly believing we can birth our babies, just as women have done for ages. The world was well-populated long before modern obstetrics, and today the lowest maternal and infant mortality and morbidity rates are in the countries where natural, midwife-assisted births are the norm.
Not only can we birth our babies naturally, we can birth in our own style. Birth doesn’t need to be performed in any specific way. It is a woman’s right to create her labor her way, and she needs to be accepted for her way of doing it. She may find help in deep breathing, light breathing, dancing, singing, yelling, screaming, moaning, crying, walking, or bathing. She needs support for whatever works to assist her to birth her baby. Soaking in water can also help tremendously in reducing pain in labor. Prenatal yoga can be extremely helpful since it teaches women to relax by using deep breathing techniques and imagery. Both of these methods help her to connect more profoundly to her body and baby.
No woman should feel like a failure for having used pain relief medication during labor. There is a time and place for it in specific circumstances, and epidurals may be very effective. However, the decision to use an epidural should be an educated one, made only after all other options have been exhausted. Birthing is hard work. It is sweaty, noisy, and emotional, and it always requires our full attention. If we accept this, and stop trying to make birthing "civilized," we can help mothers to endure and cope.
Assisting a woman who is giving birth also is hard work, requiring education, love, and our full attention. Supporting birthing women in this way results in less fear, less pain, and a decrease in the need and desire for epidural anesthesia. The satisfaction of a natural birth - including the sheer endurance of pain and sometimes overwhelming sensations - is accompanied by great joy, even ecstasy. The realization of all these complex emotions is experienced not only by the mother but also by her partner and those who assist, attend, and support her in labor. The sense of joy and accomplishment from a natural birth is the right of every woman - and a wonderful gift to any newborn in those very special, first moments of life. NOTES
1. Barbara Katz Rothman, In Labor: Women and Power in the Birthplace, (New York: W.W. Norton & Company, 1991), 80
2. Sifton, David W. Ed., The Physician’s Desk Reference (Montvale, NJ: Medical Economics Company, 1996), 2318.
3. Joseph Gambone, D.O., and Katherine Kahn, M.D., "The Effect of Epidural Analgesia for Labor on the Cesarean Delivery Rate," Obstetrics and Gynecology 83, No. 6 (June 1994):1045-1052; Thorp, M.D., et. al., "Epidural Anesthesia and Cesarean Section for Dystocia: Risk Factors in Multiparas," American Journal of Perinatology 8, No. 6: 402-410; Thorp, M.D., et. al., "The Effect of Intrapartum Epidural Analgesia on Nulliparous Labor: A Randomized, Controlled, Prospective Trial," American Journal of Obstetrics and Gynecology 169, No. 4: 851-858.
4. Author’s name, "The Bad News About Epidurals," Time, March 24, 1997, page 40.
5. Fusi, et al., "Maternal Pyrexia Associated with the Use of Epidural Analgesia in Labour," Lancet 8649 (3 June 1989): 1250.
6. B.M. Morgan, S. Rehor, and P.J. Lewis, "Epidural Anesthesia for Uneventful Labor," Anesthesia 35 (1980): 57-60.
7. Arlene Eisenberg, Heidi Murkhoff, and Sandee Hathaway, What to Expect When You’re Expecting (New York: Workman Publishing, 1984), 227.
8 Robbie E. Davis-Floyd, Birth as an American Rite of Passage (Los Angeles: University of California Press, 1992), 115. OTHER REFERENCES
Griffin, Nancy. "The Epidural Express: Real Reasons Not to Jump On Board," Mothering , Spring, 1997.
Mitford, Jessica. The American Way of Birth. Dutton, New York, 1992.
Morton, Sally, Ph.D.; Williams, Mark, M.D.; Keller, Emmett, PhD.; Peaceman, M.D., et. al., "Factors that influence route of delivery - active vs. traditional labor management," American Journal of Obstetrics and Gynecology, Vol. 169, No. 4, 940-944.
Sepkowski, Lester, Ostheimer and Brazelton. "The effects of maternal epidural anesthesia on neonatal behavior during the first month," Development of Medicine and Child Neurology, 1992, 34, 1072-1080. This article was originally edited by Leslie Hauslein. Shannon Baruth is a birth assistant, apprenticing midwife, mother to Cassidy Rose (2 1/2) and Sage (14 months), and partner to Michael. She graduated from Bryn Mawr College in 1997 with a bachelor’s degree in anthropology. She resides in rural Wisconsin. Joann Dozer is a registered nurse and CPM who has been delivering babies at home for more than 20 years. A trained Gestalt therapist, she provides counseling and workshops for women and couples. Joanne is the mother of Scott, born in 1968 in a hospital delivery that included the use of Demerol and spinal anesthesia; Lianna, born in 1973 in the birthing room of an Amish midwife’s home; and Emily, born in 1976 at home with a midwife and doctor.
Epidural Epidemic - Drugs in Labor: Are They Really Necessary. . . or Even Safe?
By Joanne Dozer and Shannon Baruth
Issue 95, July/August 1999
The use of epidurals is so common today that many perinatal professionals are calling the 1990s the age of the epidural epidemic. Believed by many in the medical profession to be safe and effective, the epidural seems now to be regarded as a veritable panacea for dealing with the pain of childbirth.
It is true that most women experience pain during the course of labor. This pain can be intense and very real, even for those who have prepared for it. But pain is only one of many possible sensations and experiences that characterize the experience of giving birth. Barbara Katz Rothman, a sociologist who studies birth in America, writes that in the medical management of childbirth, the experience of the mother is viewed by physicians as pain: pain experienced and pain to be avoided.1 Having experienced childbirth ourselves, we have great compassion for women in painful labors. However, we also feel a responsibility to mothers and their babies to explore issues concerning the use of epidural anesthesia in labor issues that are seldom discussed prenatally.
Several factors make the use of epidurals potentially hazardous. The Physician’s Desk Reference cautions that local anesthetics - the type used in epidurals - rapidly cross the placenta. When used for epidural blocks, anesthesia can cause varying degrees of maternal, fetal, and neonatal toxicity which can result in the following side effects: hypotension, urinary retention, fecal and urinary incontinence, paralysis of lower extremities, loss of feeling in the limbs, headache, backache, septic meningitis, slowing of labor, increased need for forceps and vacuum deliveries, cranial nerve palsies, allergic reactions, respiratory depression, nausea, vomiting, and seizures.2 In addition, a piece of the catheter that delivers the drug into the duraregion of the back may break off and be left in the woman, a dangerous risk that necessitates surgical removal. One of the most well-known side effects of spinal anesthesia is a spinal headache. Depending on the amount of anesthetic used and how the catheter was placed, the headache can be mild or severe, lasting between one and ten days after the birth. This is not how any of us wants to feel in our first days and hours with our newborn.
Epidurals also have been linked to an overall increase in operative deliveries: cesareans, forceps deliveries, and vacuum extractions. A meta-analysis of the effects of epidural anesthesia on the rate of cesarean deliveries was undertaken by a group of physicians who examined, categorized, and analyzed all available literature. Eight primary studies revealed that the rate of cesarean section was 10 percentage points higher in the women who had received epidural anesthesia. One study actually found that the cesarean rate increased to 50 percent when the epidural was given at 2 cm dilation, 33 percent at 3 cm, and 26 percent at 4 cm.3 What caused this increase? In the first stage of labor, the muscles of the pelvic floor may become slack from the numbing effects of the epidural, causing the baby to change an otherwise ideal position or fail to descend into the pelvic cavity. In the second stage of labor, the anesthetized woman often is unable to push effectively since she cannot feel her muscles. When the baby does not descend properly or is malpositioned, progress can slow or stop, resulting in a longer labor and the increased possibility of a cesarean section, vacuum extraction, or forceps delivery.
In addition, epidurals usually slow contractions, which prompts medical personnel to administer intravenous Pitocin in order to strengthen them and increase their frequency. Even with Pitocin, which carries its own set of risks, an anesthetized labor may remain prolonged, risking a difficult labor with lack of progress. Prolonged labors put both mother and baby at greater risk of infection, necessitating the use of antibiotics. The longer a labor and slower the progress, the more likely it will end in a forceps, vacuum, or cesarean delivery. Since cesarean section is a major surgery, it strongly influences a woman’s recovery and the initiation of breastfeeding. Of course, the rate of postpartum infection is much higher with cesarean births. All vacuum extraction and forceps deliveries increase the risk of morbidity and birth injuries.
Another effect of epidurals during labor is the creation of hypotension in the mother, which can lead to bradycardia (a decrease in the heart rate) in the fetus. All types of anesthesia, including epidurals, can negatively affect the baby’s heart rate, possibly leading to fetal distress and necessitating an operative delivery. The newborn can continue to have breathing difficulties after birth, requiring supplemental oxygen or even resuscitation. While these problems may be resolved immediately following the birth, they often require the mother to be separated from her baby for neonatal nursery observation. This separation delays bonding and initial feeding. In addition, poor muscle tone and increased acidity in the baby’s blood due to bradycardia and oxygen deprivation may affect her ability to suck effectively, hampering initial attempts at early breastfeeding.
A mother’s temperature may become elevated with the use of epidural anesthesia, resulting in the infant being taken to the nursery and given a full work-up for possible infection. This may include extensive blood work and a spinal tap.4, 5
Furthermore, though epidurals usually remove all sensation in the lower body, "windows" can occur which leave the woman experiencing the intensity of her labor (perhaps on one side of her body) but with extremely limited mobility - obviously hindering her ability to cope with her contractions.6 The idea that pain medication can play a role in "natural childbirth" is deceptive, despite the assurance of the authors of What to Expect When You’re Expecting that "...wanting relief from excruciating pain is natural...therefore pain relief medication can play a role in natural childbirth."7 This is rather twisted logic, since the concept of natural childbirth depends on the mother experiencing both mental and physical sensations of labor. The epidural may allow a woman to be awake and aware of what is happening, but she will not be experiencing a natural labor as she will be numb to any physical sensations below the waist. A split between the mind and the body is effectively created with this anesthetic, disengaging her mind from her physical feelings. Could such disconnection be natural childbirth? Robbie Davis-Floyd, an anthropologist who studies birth in America, argues that the woman in labor with an epidural "...is separated as a person as effectively as she can be from the part of her that is giving birth."8 There is an eerie quality to this kind of birth; the mother is robbed of her own connection to her power and life-creative force. She loses the opportunity to experience the inherent wisdom of the body and its ability to birth without interference. Indeed, most women who have felt childbirth agree that it was a deep, enriching, and positive experience.
What alternatives do women have for the relief of pain in labor? Unfortunately, many women enter the birth experience with a strong belief that birth is something horrible and nightmarish. They are already filled with fear, not only for their own and their baby’s safety but also about what they have heard is the unbearable pain of childbirth. Another important fear is that of "losing control" during labor and delivery. A mother often is labeled out of control if she expresses the natural, primal sounds of labor. Technologically oriented medical practitioners who are sure that childbirth is something to be wrestled into submission feel that the sound of a mother wailing in pain is a sign that she is "losing it" and ought to be medicated. In hospitals, mothers are often told by well-meaning nurses to be quiet so as not to disturb the other "patients." But release of sound is a natural way to express and release painful - and intense - sensations. Suppressing a mother’s natural instincts to move around freely and make noise in labor will increase her actual pain. The prepared childbirth movement - in particular the Lamaze technique - has been successful for some women by helping them remain "in control" by training for structured labor breathing. However, some women actually do connect to their body rhythms and natural breathing patterns in labor, and if they are more loyal to themselves than to their training, they may be seen as wild, out-of-control "Lamaze failures." This failure is defined as their inability in labor to be mannerly and controlled. In fact, one of the primary psychological reasons for lack of progress and cesareans is a fearful mother’s unconscious attempts to control the intensity of her labor. Her lack of progress is due to her inability to let go and surrender. Mothers are told they must be in control when actually they need to let go.
So how does a mother let go and find her way through the pain of labor? First, she needs to give birth where she feels safe. For some women this may mean a medicalized hospital birth; others may feel safest at home or in an alternative birthing center. Most women find that they feel safest in the loving hands of a practitioner with whom they have developed a supportive and loving relationship. This person may be a special kind of doctor or it may be a midwife. Midwives specialize in personalized, supportive perinatal care. Support is the best form and prime source of non-pharmacological pain relief. Support can also come from the love and care of a partner. If you are having your baby in a hospital, it may be worthwhile to secure the help of a knowledgeable friend or a doula. Support can be active: massage, breathing together, encouraging words and attentiveness, and reassurance that what it happening is normal and that you are handling it well. Other support can be more passive: a midwife’s calm demeanor, a gentle nurse’s presence, the peaceful attentions of loved ones. A laboring mother needs to feel safe, loved, and accepted. And when she is, whether she screams, hollers, whines, moans, bargains, begs, or just plain doesn’t act "civilized," giving birth vaginally without medication is a triumph in itself.
One of the ways to endure labor is to recognize (ideally, during one’s prenatal education) the connection between fear, tension, and pain - the "fear-tension-pain syndrome." Basically, when a mother feels fear, she will be tense and experience more pain. Relaxation relieves the tension that helps create the sensation of intense pain. The notion of a relaxing labor might seem crazy, but it is possible, and we have seen it many times. Of course, a mother will feel more relaxed and safer in the birth environment of her choice and with her chosen caregivers. Perhaps the more the mother chooses about her birth environment, the more fully she can relax.
Childbirth education classes that focus on birth as natural and normal encourage women to trust the birthing process. Birthing is full of new sensations which can be frightening and difficult to integrate; some women tell us that they felt they might split in two! Understanding the reasons behind the sensations can make them more manageable, since we fear most that which we do not understand. Another key concept in prenatal education is truly believing we can birth our babies, just as women have done for ages. The world was well-populated long before modern obstetrics, and today the lowest maternal and infant mortality and morbidity rates are in the countries where natural, midwife-assisted births are the norm.
Not only can we birth our babies naturally, we can birth in our own style. Birth doesn’t need to be performed in any specific way. It is a woman’s right to create her labor her way, and she needs to be accepted for her way of doing it. She may find help in deep breathing, light breathing, dancing, singing, yelling, screaming, moaning, crying, walking, or bathing. She needs support for whatever works to assist her to birth her baby. Soaking in water can also help tremendously in reducing pain in labor. Prenatal yoga can be extremely helpful since it teaches women to relax by using deep breathing techniques and imagery. Both of these methods help her to connect more profoundly to her body and baby.
No woman should feel like a failure for having used pain relief medication during labor. There is a time and place for it in specific circumstances, and epidurals may be very effective. However, the decision to use an epidural should be an educated one, made only after all other options have been exhausted. Birthing is hard work. It is sweaty, noisy, and emotional, and it always requires our full attention. If we accept this, and stop trying to make birthing "civilized," we can help mothers to endure and cope.
Assisting a woman who is giving birth also is hard work, requiring education, love, and our full attention. Supporting birthing women in this way results in less fear, less pain, and a decrease in the need and desire for epidural anesthesia. The satisfaction of a natural birth - including the sheer endurance of pain and sometimes overwhelming sensations - is accompanied by great joy, even ecstasy. The realization of all these complex emotions is experienced not only by the mother but also by her partner and those who assist, attend, and support her in labor. The sense of joy and accomplishment from a natural birth is the right of every woman - and a wonderful gift to any newborn in those very special, first moments of life. NOTES
1. Barbara Katz Rothman, In Labor: Women and Power in the Birthplace, (New York: W.W. Norton & Company, 1991), 80
2. Sifton, David W. Ed., The Physician’s Desk Reference (Montvale, NJ: Medical Economics Company, 1996), 2318.
3. Joseph Gambone, D.O., and Katherine Kahn, M.D., "The Effect of Epidural Analgesia for Labor on the Cesarean Delivery Rate," Obstetrics and Gynecology 83, No. 6 (June 1994):1045-1052; Thorp, M.D., et. al., "Epidural Anesthesia and Cesarean Section for Dystocia: Risk Factors in Multiparas," American Journal of Perinatology 8, No. 6: 402-410; Thorp, M.D., et. al., "The Effect of Intrapartum Epidural Analgesia on Nulliparous Labor: A Randomized, Controlled, Prospective Trial," American Journal of Obstetrics and Gynecology 169, No. 4: 851-858.
4. Author’s name, "The Bad News About Epidurals," Time, March 24, 1997, page 40.
5. Fusi, et al., "Maternal Pyrexia Associated with the Use of Epidural Analgesia in Labour," Lancet 8649 (3 June 1989): 1250.
6. B.M. Morgan, S. Rehor, and P.J. Lewis, "Epidural Anesthesia for Uneventful Labor," Anesthesia 35 (1980): 57-60.
7. Arlene Eisenberg, Heidi Murkhoff, and Sandee Hathaway, What to Expect When You’re Expecting (New York: Workman Publishing, 1984), 227.
8 Robbie E. Davis-Floyd, Birth as an American Rite of Passage (Los Angeles: University of California Press, 1992), 115. OTHER REFERENCES
Griffin, Nancy. "The Epidural Express: Real Reasons Not to Jump On Board," Mothering , Spring, 1997.
Mitford, Jessica. The American Way of Birth. Dutton, New York, 1992.
Morton, Sally, Ph.D.; Williams, Mark, M.D.; Keller, Emmett, PhD.; Peaceman, M.D., et. al., "Factors that influence route of delivery - active vs. traditional labor management," American Journal of Obstetrics and Gynecology, Vol. 169, No. 4, 940-944.
Sepkowski, Lester, Ostheimer and Brazelton. "The effects of maternal epidural anesthesia on neonatal behavior during the first month," Development of Medicine and Child Neurology, 1992, 34, 1072-1080. This article was originally edited by Leslie Hauslein. Shannon Baruth is a birth assistant, apprenticing midwife, mother to Cassidy Rose (2 1/2) and Sage (14 months), and partner to Michael. She graduated from Bryn Mawr College in 1997 with a bachelor’s degree in anthropology. She resides in rural Wisconsin. Joann Dozer is a registered nurse and CPM who has been delivering babies at home for more than 20 years. A trained Gestalt therapist, she provides counseling and workshops for women and couples. Joanne is the mother of Scott, born in 1968 in a hospital delivery that included the use of Demerol and spinal anesthesia; Lianna, born in 1973 in the birthing room of an Amish midwife’s home; and Emily, born in 1976 at home with a midwife and doctor.
Labels:
alternatives,
childbirth,
delivery,
doctors,
epidural,
labor,
management,
medication,
natural birth,
options
5.07.2010
Breastfeeding Joys
I thought today I'd share a great blog written by a friend, activist and doula. She writes on the joys of breastfeeding.
Visit her blog. She's new to this but I think you'll enjoy what she'll have to say. She is filled with warmth, knowledge and compassion.

Being a Mom of two under two can be very challenging at times. From changing diapers to cleaning banana out of the carpet, all while trying to get dinner on the table by 5 and keep up on the Laundry. There is little time to stop and take time for your self.
There seems to be only brief moments when the world comes to a halt and nothing else seems to matter. It happens a few times throughout the day as you are cleaning, cooking, or chasing your toddler. It even sometimes happens while you are running your errands. You hear a coo, or a fuss and nothing else in the world matters everything stops and its just you and your baby.
Her sweet little lips rooting for the warmth and comfort of the breast, pure satisfaction comes across her little face as she latches on. Her eyes meet yours and your heart swells with love. There is nothing more rewarding.
I have found from the first moment I held my children in my arms I knew I had to provide what was best for them. There is nothing more pure more wonderful and more loving than Breastfeeding your baby. Knowing that my body is capable of fulfilling all the needs of my infant is truly satisfying.
Visit her blog. She's new to this but I think you'll enjoy what she'll have to say. She is filled with warmth, knowledge and compassion.
Joys of Nursing

Being a Mom of two under two can be very challenging at times. From changing diapers to cleaning banana out of the carpet, all while trying to get dinner on the table by 5 and keep up on the Laundry. There is little time to stop and take time for your self.
There seems to be only brief moments when the world comes to a halt and nothing else seems to matter. It happens a few times throughout the day as you are cleaning, cooking, or chasing your toddler. It even sometimes happens while you are running your errands. You hear a coo, or a fuss and nothing else in the world matters everything stops and its just you and your baby.
Her sweet little lips rooting for the warmth and comfort of the breast, pure satisfaction comes across her little face as she latches on. Her eyes meet yours and your heart swells with love. There is nothing more rewarding.
I have found from the first moment I held my children in my arms I knew I had to provide what was best for them. There is nothing more pure more wonderful and more loving than Breastfeeding your baby. Knowing that my body is capable of fulfilling all the needs of my infant is truly satisfying.
5.03.2010
Kids Things Say
Yes, you read that right. The title is fitting, since many times, our toddlers try so hard to imitate what they've heard from us and use it in context, but usually miss one or two things in the process.
Alexander is at that fun stage where his vocabulary is taking off but it his thought process hasn't quite caught up. His new favorite phrase is "Told you! Haha" but he uses it at the most random and inappropriate times. Of course, this just makes it funny and adorable.
What are some cute and crazy things your kids are saying (or have said)?
I love to hear all the funny (or embarrassing) stories!
Alexander is at that fun stage where his vocabulary is taking off but it his thought process hasn't quite caught up. His new favorite phrase is "Told you! Haha" but he uses it at the most random and inappropriate times. Of course, this just makes it funny and adorable.
What are some cute and crazy things your kids are saying (or have said)?
I love to hear all the funny (or embarrassing) stories!
Subscribe to:
Posts (Atom)









